On Thursday, US officials granted final approval to a highly-anticipated Alzheimer's drug, paving the way for Medicare and other insurance plans to begin covering the treatment for patients suffering from the degenerative brain disease.
The Food and Drug Administration has approved the intravenous drug Leqembi for patients with moderate dementia and other early Alzheimer's disease-related symptoms. It is the first drug that has been demonstrated to reduce the cognitive decline of Alzheimer's patients moderately.
FDA Grants Full Approval to New Alzheimer's Medicine
In January, the FDA granted Eisai conditional approval for its Alzheimer's disease drug Leqembi based on preliminary data indicating that it worked by removing an adhesive brain plaque linked to the disease.
The FDA confirmed these findings by analyzing data from a larger, 1,800-patient study that demonstrated the drug delayed memory and cognitive decline by approximately five months in those who received the treatment versus those who received a placebo.
The most severe type of warning will be included in the drug's prescribing information, indicating that Leqembi can rarely cause hazardous adverse effects such as cerebral swelling and bleeding. The label indicates that these side effects are observed with other Alzheimer's medications that target plaque, CBS News reported.
Typically, converting a substance to FDA approval receives little attention. However, Alzheimer's patients and advocates have been lobbying the federal government for months after Medicare officials announced last year that they would not cover the routine use of Leqembi until the drug received FDA approval.
It was feared that the cost of new Alzheimer's medicines that target plaque, such as Leqembi, could overwhelm the program's finances, which provide treatment for 60 million seniors. Leqembi costs approximately $26,500 for a one-year supply of IV infusions every two weeks.
Most Alzheimer's patients in the United States are covered by Medicare. And private insurers have followed suit, withholding coverage for Leqembi and a comparable drug, Aduhelm, until they receive FDA approval. A decision regarding Aduhelm's comprehensive FDA approval is still years away.
The administrator of Medicare, Chiquita Brooks-LaSure, has cleared that the program will begin paying for the drug immediately following FDA approval. However, the government also imposes additional requirements.
Beneficiaries of Medicare who receive Leqembi must enroll in a federal registry to monitor the drug's real-world safety and efficacy. Medicare officials stated that the information will advance "knowledge of how these drugs can potentially assist individuals."
Ivan Cheung, Americas region chairman and CEO of Tokyo, Japan-based Eisai, referred to the FDA's approval of Leqembi as a "victory for the Alzheimer's disease community" because it is the first drug to halt the progression of the disease.
Read Also : Ohio Man Gets Life Sentence for Raping Girl Who Drew National Attention Over Getting Legal Abortion
Alzheimer's Drug Leqembi has Side Effects
Per USA Today, the FDA will require a boxed warning regarding the drug's known adverse effects, which include cerebral edema and small bleeding. Some patients who take Leqembi or other amyloid-targeting medications develop these adverse effects, known as amyloid-related imaging abnormalities.
While most patients will not experience early-onset symptoms, some may experience migraines or infusion-related reactions such as fever, chills, or gastrointestinal distress.
The safety language warns that "rarely, life-threatening events can occur," which includes strokes. Patients who inherited two copies of the Alzheimer's risk gene ApoE4 have an increased risk of edema and brain bleeding, according to the warning language.
Approximately 15% of patients who take the medication have two copies of this susceptibility gene. Before beginning treatment, patients should undergo a genetic test to determine their ApoE4 status, according to the safety warning.
The FDA also suggests that physicians discuss genetic testing with their patients. If patients decline testing, physicians cannot determine whether they have a higher genetic risk of cerebral swelling and hemorrhage.
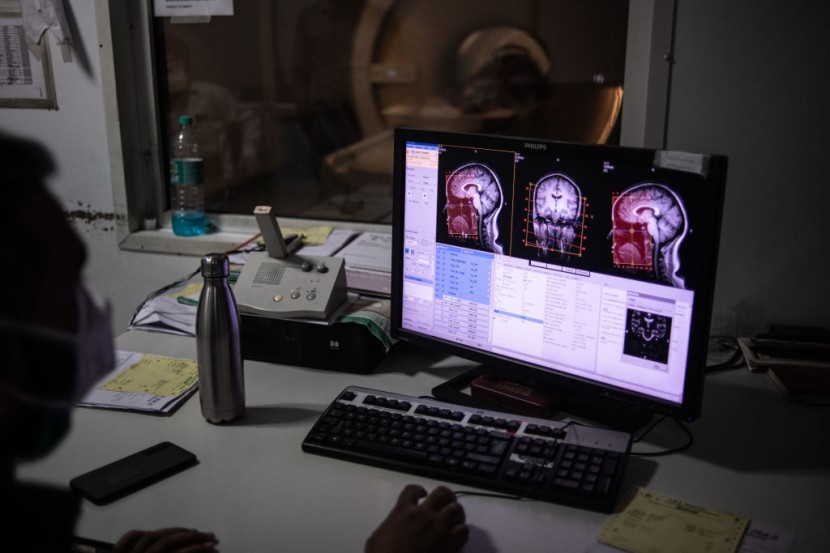
The FDA advised doctors to be circumspect when prescribing the drug to patients taking blood thinners. Before administering the drug, physicians must validate the presence of amyloid in the patient's brain using a PET scan or spinal tap.
During the first year of treatment, patients must also undergo multiple MRIs to check for adverse effects.
Related Article : America's 'Zombie Drug' Tranq Death Cases Now 34x Higher! Is UK Next?








