Two consumer advocacy groups have taken a significant step by filing a lawsuit in a Florida federal court to halt the state's termination of residents' Medicaid benefits.
This lawsuit marks a notable development as it becomes the first in the nation to challenge the resumption of Medicaid eligibility reviews and the subsequent dropping of enrollees who are deemed ineligible, according to CNN.
Lawsuit Challenges Medicaid Benefit Termination
This process, which Congress had suspended for three years during the COVID-19 pandemic, has been reinstated, with various states restarting as early as April.
The Florida Health Justice Project and the National Health Law Program jointly filed the lawsuit on behalf of three Floridians in the US District Court in Jacksonville.
The plaintiffs include a 25-year-old woman and her 2-year-old daughter with cystic fibrosis, as well as a 1-year-old girl. The lawsuit specifically targets the state's Agency for Health Care Administration and the Department of Children and Families.
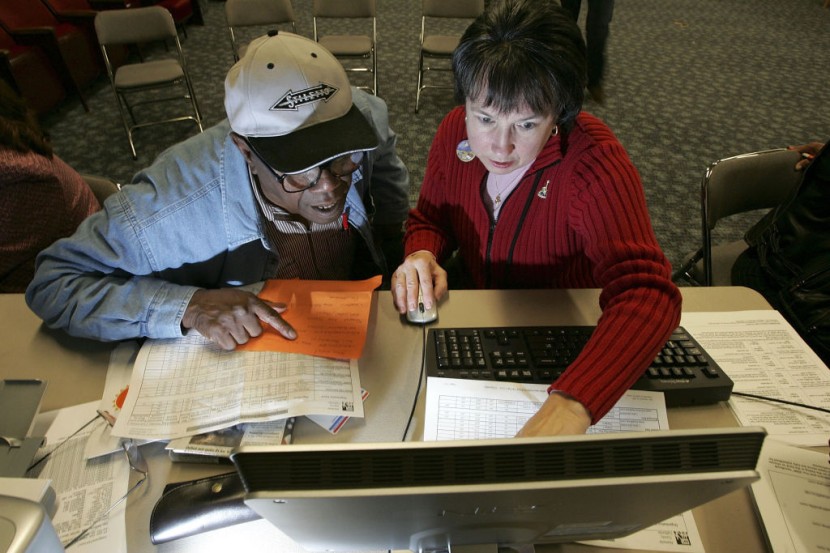
Central to the lawsuit's argument is the contention that the notices being sent by these agencies to inform enrollees about the loss of their eligibility are both confusing and insufficient in explaining the reasons behind the termination of coverage.
The plaintiffs claim that this lack of clarity hampers their ability to understand the agencies' decisions, contest the loss of coverage, and plan for a smooth transition that minimizes disruptions in necessary medical care.
The lawsuit seeks to compel the court to require the state to cease terminating enrollees until they can provide adequate notice and the opportunity for a pre-termination fair hearing.
The plaintiffs, through their advocacy groups, aim to ensure that individuals are not left without essential healthcare coverage due to a lack of clear communication.
Mallory McManus, Deputy Chief of Staff for the Department of Children and Families, dismissed the lawsuit as baseless and emphasized that the letters sent to recipients are "egally sufficient. McManus also pointed out that the federal Centers for Medicare and Medicaid Services had approved the Department's redetermination plan, based on regulatory guidelines.
However, advocates stress that the consequences of inadequate communication can be severe, impacting access to crucial medical services. Without Medicaid coverage, individuals may face difficulties obtaining prescription drugs, children's vaccinations, and post-partum care, leading to potential disruptions in their healthcare journey.
The lawsuit underscores broader concerns about the Medicaid eligibility review process taking place across the United States, as per The Hill.
Delving Into the Challenges of Healthcare Access
In Florida alone, nearly 183,000 residents have received notices stating that they no longer qualify for Medicaid coverage. Furthermore, hundreds of thousands more are expected to undergo coverage reviews in the upcoming year.
Notably, a significant portion of individuals, approximately 226,000, have been dropped from Medicaid for procedural reasons, often due to difficulties in completing renewal applications. This can occur when renewal notices are sent to outdated addresses, are poorly understood, or are not returned within the required timeframe.
Across the nation, the phenomenon of "Medicaid unwinding" has led to over 5.2 million individuals being disenrolled since the spring. Alarmingly, the majority of those who have lost their coverage were dropped for procedural reasons, highlighting the complexities and potential pitfalls within the system.
This lawsuit in Florida serves as a microcosm of the larger challenges surrounding healthcare access and eligibility determination for vulnerable populations. As the legal battle unfolds, it prompts reflection on the importance of transparent and effective communication in the administration of public healthcare programs.
The outcome of this case will likely reverberate beyond Florida, shaping the ongoing conversation about how to strike a balance between eligibility reviews and ensuring that individuals receive uninterrupted access to essential medical services, US News reported.
© 2025 HNGN, All rights reserved. Do not reproduce without permission.